Episodic Care Demands Specialized Coding Expertise
When it comes to urgent care billing services and emergency medical billing, coding is not just a backend task—it’s a frontline defense for revenue. Unfortunately, many facilities rely on generalist coders who lack the training to handle high-stakes, episodic care environments.
Emergency departments and urgent care centers face complex, fast-moving scenarios—ranging from trauma activations to critical care procedures and higher-level E/M services. These encounters require coders who know exactly what to look for, or valuable revenue will be left unbilled or undercoded.
The High Stakes of Inexperienced Coding
Using coders without episodic care experience leads to:
- Missed trauma and critical care charges
- Incorrect E/M level selection
- Incomplete documentation reviews
- Higher denial rates and compliance risks
Even small mistakes can trigger audits, delays, or lost revenue. In an environment where time equals money, accuracy is everything.
How 360’s Contracted Coders Close the Gap
At 360 Medical Billing Solutions, we partner with certified coders who are experienced specifically in emergency and urgent care environments. These professionals understand the intricacies of episodic services and are trained to:
- Identify all billable services within chaotic clinical notes
- Apply CPT, ICD-10, and HCPCS codes accurately under pressure
- Review documentation to ensure NSA and EMTALA compliance
- Work seamlessly with HL7 interfaces to catch missing charts or mismatched codes
When supported by real-time data from HL7-integrated systems, our coding partners are better equipped to ensure complete and accurate charge capture across emergency and urgent care encounters.
FAQs
Why not use in-house coders for urgent care billing services?
In-house coders may not have episodic care experience or may be stretched too thin to ensure accuracy under volume pressures.
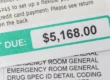
Can incorrect coding really impact collections?
Yes. It can lead to undercoding (lost revenue), overcoding (compliance risk), or denials (payment delays).
What should I look for in a contracted coder?
Experience with emergency/urgent care, coding certification, strong knowledge of payer policies, and familiarity with HL7-integrated systems.
Why 360 Medical Billing Solutions Is Your Best Partner
Whether you’re managing a freestanding ER or a busy urgent care clinic, accurate coding is essential to revenue and compliance. 360 ensures that only specialized, vetted coders work on your claims—so you get paid what you deserve, without delays or risks.
- No hidden costs
- Little to no out-of-pocket initial costs
- Access to coders with trauma, E/M, and urgent care expertise
- Seamless integration with HL7 healthcare data systems